WHAT IS A VASECTOMY REVERSAL?
Approximately 6% of men who have had a vasectomy request a vasectomy reversal.
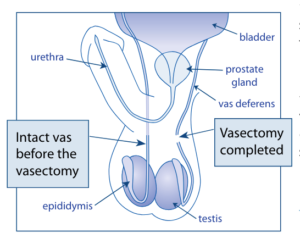
A vasectomy reversal involves finding and re-joining the previously divided ends of the vas deferens (tube that delivers sperm from the testes). Unfortunately, the procedure for reversal is much more complicated than the initial vasectomy.
The procedure is usually done as a day case, under a general anaesthetic, and takes several hours. Because the vas deferens is a fine structure, <5mm in diameter, it is more challenging to reconstruct. Best results are obtained using a surgical microscope and fine sutures, which are thinner than a human hair.
A small incision is made in the scrotum to gain access to the previously cut ends of the vas deferens. Each end is secured and carefully prepared for reconstruction. Non dissolvable sutures are used to reconstruct the vas deferens, but dissolvable sutures are used to close the skin. A supportive dressing is applied at the end.
HOW SUCCESSFUL IS VASECTOMY REVERSAL?
There are 2 outcomes of success to consider. The first, and the most accepted definition of success, is return of sperm to the ejaculate. The second outcome to consider is pregnancy. Rates of return of sperm to the ejaculate are always higher than rates of pregnancy. Return of sperm to the ejaculate is more likely if the vasectomy was only a few years ago and only a short segment of vas was removed. Generally, the rate of return of sperm to the ejaculate is 70-90+% depending on time since vasectomy.
Sometimes the two cut ends of the vas cannot be brought together or are not healthy enough to be joined. In this case the end of the vas may be joined directly to the epididymis (structure behind the testicle which sperm pass through). This is a more challenging procedure with lower success rates. Any post operative complications such as significant bleeding or swelling also affect success rates.
WHAT CAN I EXPECT AFTER THE PROCEDURE?
- Bruising and swelling of the scrotum – this is common. Tight underwear and scrotal elevation using a rolled-up tea towel will help limit swelling – similar to elevating an injured ankle. You may find ice packs helpful to reduce pain and swelling in the first few days after surgery (but do not apply them directly to your skin).
- Avoid public swimming pools or prolonged hot showers/baths for 2 weeks.
- You will be asked to obtain a semen analysis around 6 weeks post-surgery. This will usually be repeated at 3 months post-surgery as that is how long it takes to make new sperm.
WHAT ABOUT EXERCISE/ACTIVITY?
- Refrain from heavy lifting or strenuous activity for at least 2 weeks to allow adequate healing and recovery.
- You can return to sexual activity at 4 weeks.
WHAT ABOUT MEDICATION?
WHAT ARE THE POSSIBLE COMPLICATIONS?
- Bruising/bleeding into the scrotum
- Infection
- Inadvertent damage to the testicle, epididymis or vas deferens
- Chronic pain
- Failure to achieve return of sperm to the ejaculate
NOTIFY GM UROLOGY or your GP if you experience any of the following:
- Heavy bleeding from the incision
- Increasing swelling of the scrotum or swelling around the surgical sites
- Increasing pain
- Redness spreading from incision points
- Fever (with a temperature of more than 37.5 degrees) or chills
- Any other concerns regarding your surgery



