WHAT IS A PYELOPLASTY?
A Pyeloplasty is a surgical procedure on the renal pelvis in the kidney to treat PUJ (Pelvo-Ureteric junction obstruction), a condition which can cause symptoms and long-term complications.WHAT IS THE PUJ?
This stands for Pelvo-Ureteric Junction. This is where the renal pelvis joins the upper end of the ureter, the tube through which urine flows from the kidney to the bladder. The renal pelvis is a funnel shape that has cup like extensions, called Calyces, within the kidney. Under normal conditions, the kidneys filter the blood and remove waste, salts and water to produce urine. This collects in the renal pelvis before it flows on through the ureter into the bladder.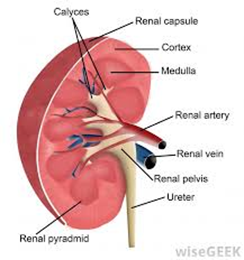
WHAT IS A PUJ OBSTRUCTION AND WHAT ARE ITS CONSEQUENCES?
An obstruction of the PUJ is when the kidney makes urine faster than it can be drained through the renal pelvis into the ureter. This causes the urine to pool in the kidney, which leads to kidney swelling (Hydronephrosis).
This can cause symptoms such as flank pain, recurrent infections, blood in urine (haematuria) and lead to complications including loss of kidney function and kidney stones.
The cause of a PUJ obstruction can either be primary (congenital) – due to deficiency of muscle in the PUJ or a blood vessel crossing the PUJ. It can also be secondary, such as a stricture from a stone, previous surgery or tumour.
Once secondary causes have been ruled out, the diagnosis of PUJ obstruction is made with imaging including a renogram (MAG3 or DTPA). Treatment is only recommended if the PUJ obstruction is confirmed and is causing symptoms or complications. This is usually in the form of a pyeloplasty.
HOW IS A PYELOPLASTY PERFORMED AND WHAT CAN I EXPECT POST-OP?
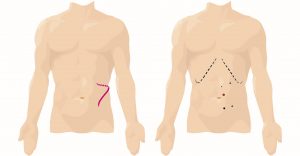
The operation is performed using 4-5 “keyholes” and using the latest da Vinci® Xi robotic surgical system.
- Less pain
- Less blood loss
- Shorter length of stay (1-2 days)
- Faster recovery to normal activities (1-2 weeks)
- Faster return to work (2-6 weeks depending on occupation)
- Better dexterity for suturing during the procedure
WHAT ABOUT DIET?
- Drink plenty of fluids (8-10 glasses or 2-3 litres)
- Ensure adequate nutrition to improve healing. You may need to have 6 smaller meals rather than 3 larger ones.
- Eat a diet high in fibre to prevent constipation and the need for straining when using your bowels
- Take laxatives (eg. coloxyl and lactulose) as directed
WHAT ABOUT EXERCISE/ACTIVITY?
- You can do gentle exercise such as walking less than 1.5km
- Avoid strenuous activity, heavy lifting (>3kg) or engage in sports (eg. golf) for 6 weeks to prevent wound complications such as hernias
- Avoid driving a car until you have no pain and not on any pain killers (about 2 weeks)
- Returning to work depends on the physical demands of your duties. You may be able to return to low physical activity jobs (eg. office work) within 3-4 weeks. You may need 6-12 weeks off jobs involving heavy manual work.
- Avoid overseas travel for 6 weeks (inform your Doctor if you have a trip planned)
WHAT ABOUT MEDICATIONS?
- You can resume your usual medications
- If your blood thinning medication was stopped, your Doctor will let you know when to recommence
- You can take 1-2 paracetamol every 4-6 hours for pain and discomfort (no more than 8 in a day)
- Stronger pain medications may also have been prescribed and should be taken as directed. Their use should decrease every day, as taking them in the long term will often cause side effects such as constipation.
WHAT ARE THE POSSIBLE COMPLICATIONS?
- Bleeding requiring blood transfusion(s)
- Infection (urine, wound, intra-abdominal, lung)
- Urine leak through anastomosis (reconstructed join between ureter and renal pelvis)
- Wound infection / hernia
- Failure of procedure to fix obstruction or relieve symptoms including pain
- Need for further operations
- Injury to blood supply of the kidney resulting in loss of this kidney
- Injury to surrounding organs (bowel, liver, spleen, pancreas, blood vessels)
- Anaesthetic / peri-op – heart attack, stroke, blood clots in the legs going to lungs.
NOTIFY GM UROLOGY or your GP if you experience any of the following:
- Increased discomfort, severe abdominal pain or bloating
- Vomiting
- Fevers (temperatures over 37.5 degrees), sweats or shakes
- Bleeding in the urine accompanied by a fever
- Increased discomfort, severe pain and burning when passing urine
- Heavy bleeding – urine looks like pure blood
- Clots causing difficulty passing urine
- Unable to pass urine
- Cloudy or offensive urine
- Increased pain, redness or purulent discharge from any of the wounds



