A “robotic assisted radical prostatectomy” (RARP) is a surgical procedure used to treat localised (not metastatic) prostate cancer using the latest technology, which has multiple benefits for the patient. The aim of this operation is to remove the entire prostate gland, the attached seminal vesicles (a pair of glands that produce part of the semen) and part of the vas deferens (the muscular cord that pumps sperm from the testicles to the urethra). In addition, depending on the risk of the cancer, local pelvic lymph nodes may also be removed with a “Pelvic Lymph Node Dissection” (PLND).
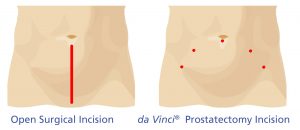
The operation is performed using “keyholes” and using the latest da Vinci® Xi robotic surgical system.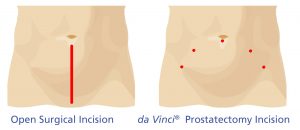
The benefits of the robotic approach include:
- Less pain
- Less blood loss
- Shorter length of stay (1-2 days)
- Faster recovery to normal activities (1-2 weeks)
- Faster return to work (2-6 weeks depending on occupation)
- Possibly improved oncological (cancer control) and functional (continence and erectile) outcomes
WHAT DOES THE PROCEDURE INVOLVE?
Once the anaesthetic is delivered the patient, asleep, is placed on the operating table and prepped. A catheter is placed into the bladder. “Keyhole” incisions are made in a line around the level of the belly button, to allow insertion of hollow tubes (cannulas) into the abdomen. Gas is then pumped into the abdomen to obtain a good view of the pelvis. The robot arms are then “docked” (attached) to these cannulas and instruments which will be used to perform the procedure are inserted. The surgeon then controls the instruments remotely (via the “surgical console”) to complete the operation. A surgical assistant and scrub nurse assist at the bedside with changing instruments and inserting/removing sutures.

 Once the prostate is disconnected, the bladder is sutured to the urethra (water pipe) over a new catheter, the robot is “undocked”, the prostate is removed via one of the keyhole incisions and the wounds are closed with absorbable sutures. The prostate and any other tissue removed are sent to the laboratory to be analysed to assess the extent of the cancer by a specialist pathologist. The patient generally wakes up a soon after the procedure in recovery, and if stable goes to the surgical ward.
Once the prostate is disconnected, the bladder is sutured to the urethra (water pipe) over a new catheter, the robot is “undocked”, the prostate is removed via one of the keyhole incisions and the wounds are closed with absorbable sutures. The prostate and any other tissue removed are sent to the laboratory to be analysed to assess the extent of the cancer by a specialist pathologist. The patient generally wakes up a soon after the procedure in recovery, and if stable goes to the surgical ward.


NERVE SPARING
A nerve sparing approach to a radical prostatectomy may be offered in some men undergoing this surgery. Whether a nerve spare is attempted depends on the man’s pre-operative erectile function and if he is sexually active as well as the extent and risk of the cancer as determined by the PSA, rectal examination, MRI and biopsy results. A nerve sparing technique involves peeling the layers off one or both sides of the prostate (like an onion) which contain nerves that enable erections, and leaving them behind whilst removing the remainder of the prostate. The risk of performing a nerve spare is getting too close to the cancer, resulting in a positive surgical margin.
Men who have a nerve sparing procedure have a greater chance of recovering their erections. The success rate also depends on the man’s age, and baseline (pre-operative) erectile function. Please ask your doctor if you would be a candidate for nerve sparing with your radical prostatectomy.
HOW DO I PREPARE BEFORE MY PROCEDURE?
- Pelvic floor exercises – commencing training your pelvic floor muscles before your surgery can improve continence recovery post-op. You will have received a referral to a physiotherapist to assess and educate you about performing pelvic floor muscle exercises. These muscles are the ones used to stop your urinary stream midway. Exercises involve contracting these muscles for 10 seconds, 10 times in a row, 3 times per day.
- Appointment with clinical nurse specialist – you will have a 1-hour appointment with our practice nurse to discuss in detail your upcoming surgery, pre-operative investigations (blood and urine tests, ECG), admission instructions, what to expect following the operation as well as address any of your concerns.
- Blood thinners – these include aspirin, clopidogrel (Plavix), warfarin, rivaroxaban (Xarelto), apixaban (Eliquis), dabigatran (Pradaxa) and need to be stopped 2-10 days prior to your surgery. Your doctor will advise you further about this.
- Other regular medications – you can take all of these, up to and including the day of your surgery, unless otherwise instructed by your doctor.
- Fasting and admission – the hospital will call you the day prior to give you fasting instructions and when/where to come into hospital (please click here for contact details in the event you do not receive this call)
WHAT CAN I EXPECT IN HOSPITAL AFTER THE PROCEDURE?
- A drain tube coming out of the abdomen connected to a collection bag (this is used to monitor for bleeding and urine leak and is usually removed the next day)
- A urinary catheter. This is attached to a leg bag on the first day post-operatively and usually stays in for 1 week (ie. you go home with it).
- Lower abdominal pain especially with moving/coughing. You will have some regular pain relief charted, but if needed please ask the nurse looking after you for extra pain killers. You may have a PCA (patient controlled analgesia) for 24 hours, which is essentially a button you press when you need some pain relief. The aim is not to be pain free but to reduce pain levels in order to ensure you pain is under control so that you are able to take deep breaths and cough.
- Gas under the skin (like bubble wrap) and bloating – this normal and should resolve within a few days
- Shoulder tip pain is common and as a result of gas irritating the diaphragm
- You will be allowed to have fluids as soon as you are alert after your operation and in most cases be able to eat food the day after
- Nausea is common for the first 24 hours after anaesthetic and treated with anti-nausea medications if required.
- Your bowels may be sluggish and not open for a few days, but as long as you are tolerating oral intake and passing wind, there is no need to be concerned.
The aim before discharge is for you to be able to:
- Tolerate a normal diet without nausea
- Pass wind through the back passage
- Pain be under control with tablets
- Be able to transfer in and out of bed and walk around
- Know how to look after your catheter at home and self-administer clexane injections (if required)
WHAT CAN I EXPECT AFTER I AM DISCHARGED?
- A date/plan for catheter removal (about 1 week) – for more information about managing your catheter at home please click here
- A follow-up appointment for you to see your doctor (in 2-3 weeks)
- Pain should decrease day by day and need for pain killers should also reduce
- Bowels should start working as normal (see below about diet)
- Wound care – you will have waterproof (ie. shower as normal) dressings and steri-strips over your wounds. These can be removed and checked around the time of your catheter removal (roughly 1 week after the surgery). The sutures are all absorbable and do not need to be removed.
WHAT ABOUT DIET?
- Drink plenty of fluids (8-10 glasses or 2-3 litres)
- Ensure adequate nutrition to improve healing. You may need to have 6 smaller meals rather than 3 larger ones.
- Eat a diet high in fibre to prevent constipation and the need for straining when using your bowels
- Take laxatives (eg. coloxyl and lactulose) as directed
WHAT ABOUT EXERCISE/ACTIVITY?
- You can do gentle exercise such as walking less than 1.5km
- Avoid strenuous activity, heavy lifting (>3kg) or engage in sports (eg. golf) for 6 weeks to prevent wound complications such as hernias
- Avoid driving a car until you have no pain and not on any pain killers (about 2 weeks)
- Avoid activities which put pressure on the perineum such as bike riding, motorcycling or horse riding for 3 months unless otherwise instructed by your doctor
- Returning to work depends on the physical demands of your duties. You may be able to return to low physical activity jobs (eg. office work) within 3-4 weeks. You may need 6-12 weeks off jobs involving heavy manual work.
- Avoid overseas travel for 6 weeks (inform your Doctor if you have a trip planned)
WHAT ABOUT MEDICATIONS?
- You can resume your usual medications
- If your blood thinning medication was stopped, your Doctor will let you know when to recommence
- You can take 1-2 paracetamol every 4-6 hours for pain and discomfort (no more than 8 in a day)
- Stronger pain medications may also have been prescribed and should be taken as directed. Their use should decrease every day, as taking them in the long term will often cause side effects such as constipation.
- If you had a nerve sparing operation, you may be prescribed tablets to help with rehabilitation of your erections, to commence taking after your catheter is removed.
WHAT ARE THE POSSIBLE SIDE EFFECTS/COMPLICATIONS?
Expected/Common
- No semen produced during ejaculation (can still have normal orgasm) causing subfertility
- Erectile dysfunction (depends on nerve sparing)
- Urinary incontinence (temporary) – improves up to 12 months post-operatively
Occasional/Uncommon
- Bleeding – requiring blood transfusion or repeat surgery
- Urine infection
- Wound infection
- Cancer cells discovered outside prostate – managed with observation or may require further treatment (eg. radiotherapy or hormone therapy)
- Urine leak – usually managed with prolonged period with drain and/or catheter
- Ileus – slowing of bowels causing vomiting and constipation
- Urinary incontinence (permanent) – requiring long term pads or further surgery Rare
- Anaesthetic, cardiovascular or perioperative problems possibly requiring intensive care admission (including chest infection, pulmonary embolus – blood clot in lungs, deep vein thrombosis – blood clot in leg, stroke, heart attack and death)
- Hernia involving any of the wounds requiring further treatment
- Injury to bowel (eg. rectum) during surgery or development of fistula between bladder and bowel possibly requiring temporary colostomy (bag)
NOTIFY GM UROLOGY or your GP if you experience any of the following:
- Catheter not draining or heavy bleeding/clots seen in catheter bag
- Increased pain, redness or purulent discharge from any of the wounds
- Increased discomfort, severe abdominal pain or bloating
- Vomiting
- Difficulty passing urine or worsening burning after catheter removed
- Fever (temperature over 37.5 degrees), chills, shakes or feeling generally unwell
FOLLOW UP APPOINTMENT
You should have an appointment to have your catheter removed (usually 1 week) and another with your doctor in 2-3 weeks. If these appointment times are not given to you on discharge from hospital, please phone GM Urology.
If you have any queries please contact GM Urology on 03 5201 7000 during business hours OR leave a message on the After Hours Urology Paging Service 03 9387 1000



